During a medical crisis, family members frequently are called upon to make decisions quickly on whether to withhold or provide life-sustaining treatments. You may already have a durable power of attorney for health care—a legal document that allows your designated agent or proxy to make medical decisions for you, if you become incapacitated. However, the instructions in a living will can be used only when the person named in the living will has no prospect of recovery or cure.
Forbes recent article entitled “How Does A Living Will Work?” says that adding a living will to your estate plan can mean the difference between your family having questions later or knowing they made the right decision for you, when you were unable to make end-of-life medical decisions for yourself.
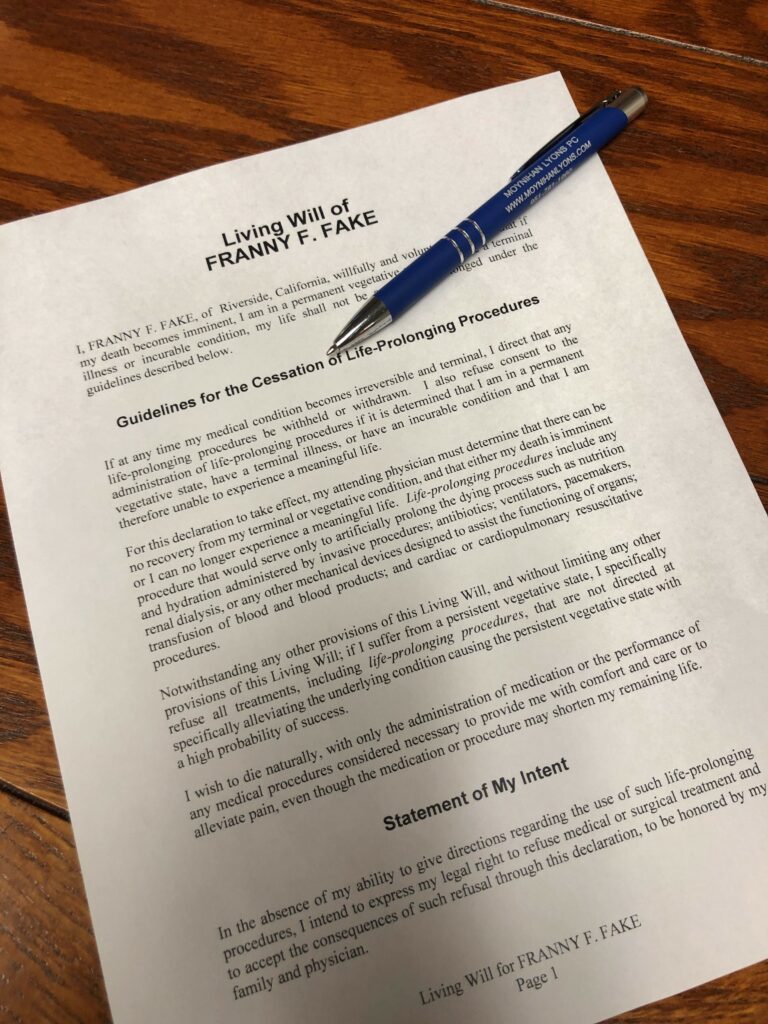
A living will is a legal document that states your wishes on receiving or declining medical care or life-sustaining treatments in the event you become terminally ill or injured and unable to communicate those decisions for yourself. The person named in the living will is known as the principal or declarant.
The document should include your wishes for receiving or going without treatment when your condition isn’t expected to improve and treatment would extend your life for only a limited time.
The living will is designed to apply only in very limited situations when the principal is so terminally ill that the principal will likely die within a short period of time. Life-sustaining treatments discussed in a living will may include:
- Artificial nutrition (via feeding tube)
- Artificial hydration (via feeding tube or IV)
- Heart-lung machines
- Dialysis
- Ventilators
- Cardio-pulmonary resuscitation (CPR); or
- Other extraordinary measures.
Living wills can also detail issues like pain management and palliative care and can even include provisions like “I would prefer to die at home.”
Reference: Forbes (Aug. 18, 2022) “How Does A Living Will Work?”